Regardless of whether the syndrome of acute HIV infection is recognized or not, after the HIV-specific immunological response begins to control the intensity of viremia, a so-called “viral set point” is established which varies by individual. With exceedingly rare exceptions, the immunological response to HIV does not eliminate infection, but rather establishes steady state between viral replication and elimination. A variable level of viremia is attained that can be measured via quantification of the number of copies of HIV RNA present in blood (viral load). Although the viral load within the first 120 days of HIV infection is not of prognostic value, most patients establish a relatively stable viral load after recovering from acute infection, and this viral set point is highly predictive of the rate of future progression of illness. In the case of a high viral load set point (i.e., values ranging up from 40000 copies/mm3), more rapid decline in CD4 cell counts and more rapid occurrence of Clinical Class B and C conditions will occur. Some patients have low viral load set points (below 500 copies/mm3), which indicates a better prognosis; no evidence of progression (CD4 cell depletion or HIV diseases) is seen for long periods of time in a small subset of patients (see section on long-term progression, below). The viral set point is likely influenced by several factors such as presence of other infections at the time of HIV exposure, genetic characteristics (particularly the type of HIV binding receptors present on lymphocytes), viral characteristics, age, and perhaps sex (see below) (Kahn, 1998).
During the period of clinical stability, acute illnesses and other events that can stimulate the immune system, such as influenza, Herpes simplex outbreaks, tuberculosis, and even routine vaccinations, have resulted in 10–1000-fold increases in viral load; these increases are transient and most often resolve within 2 months (Stanley, 1996). Thus, determination of viral load for prognostic purposes should not be done during or shortly after an acute illness.
The rules of medicine and surgery
Monday, July 26, 2010
Acute HIV infection
, Acute HIV infection is a transient symptomatic illness that can be identified in 40–90% of cases of new HIV infection. It is characterized by a high rate of HIV replication, high titers of virus in blood and lymphoid organs (up to several million copies of HIV RNA per cubic millimeter of plasma), and initiation of an HIV-specific immune response. The amount of virus present in blood and tissues begins to fall after the appearance of cytotoxic (“killer”) lymphocytes that specifically react with HIV antigens; the vigor of this response varies among individuals and is associated with subsequent rate of disease progression . A pool of persistently infected CD4 cells (“latent reservoirs”) emerges early in the course of HIV infection and persists indefinitely .
Symptoms have been identified 5–30 days after a recognized exposure to HIV .The signs and symptoms of acute HIV infection are not specific; fever, fatigue, rash, headache, homeopathy, pharyngitis, mild
 gastrointestinal upset, night sweats, aseptic meningitis, and oral ulcerations are most frequently reported. Because the clinical signs of acute HIV infection resemble those of many acute viral illnesses, the correct diagnosis is often missed. Because early treatment at the time of acute infection is actively being investigated (Rosenberg, 2000) (see Chapter IV on Primary Medical Care), early suspicion of and evaluation for HIV infection should be encouraged .
gastrointestinal upset, night sweats, aseptic meningitis, and oral ulcerations are most frequently reported. Because the clinical signs of acute HIV infection resemble those of many acute viral illnesses, the correct diagnosis is often missed. Because early treatment at the time of acute infection is actively being investigated (Rosenberg, 2000) (see Chapter IV on Primary Medical Care), early suspicion of and evaluation for HIV infection should be encouraged .
Symptoms have been identified 5–30 days after a recognized exposure to HIV .The signs and symptoms of acute HIV infection are not specific; fever, fatigue, rash, headache, homeopathy, pharyngitis, mild
 gastrointestinal upset, night sweats, aseptic meningitis, and oral ulcerations are most frequently reported. Because the clinical signs of acute HIV infection resemble those of many acute viral illnesses, the correct diagnosis is often missed. Because early treatment at the time of acute infection is actively being investigated (Rosenberg, 2000) (see Chapter IV on Primary Medical Care), early suspicion of and evaluation for HIV infection should be encouraged .
gastrointestinal upset, night sweats, aseptic meningitis, and oral ulcerations are most frequently reported. Because the clinical signs of acute HIV infection resemble those of many acute viral illnesses, the correct diagnosis is often missed. Because early treatment at the time of acute infection is actively being investigated (Rosenberg, 2000) (see Chapter IV on Primary Medical Care), early suspicion of and evaluation for HIV infection should be encouraged .
AIDS PROGRESSION
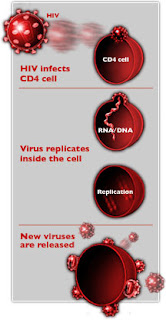 HIV infects and induces cell death in a variety of human cell lines. T-helper lymphocytes (also known as CD4 cells) are a major target of viral infection, and circulating CD4 cells become steadily depleted from peripheral blood in most untreated infected persons.
HIV infects and induces cell death in a variety of human cell lines. T-helper lymphocytes (also known as CD4 cells) are a major target of viral infection, and circulating CD4 cells become steadily depleted from peripheral blood in most untreated infected persons.Untreated HIV infection is a chronic illness that progresses through characteristic clinical stages; AIDS is an endpoint of HIV infection, resulting from severe immunologic damage, loss of an effective immune response to specific opportunistic pathogens, and tumors. AIDS is diagnosed by the occurrence of these specific infections and cancers or by CD4 cell depletion to less than 200/mm3.
TRNSMISSION OF HIV
HIV is transmitted by three primary routes: sexual, parenteral (blood-borne), and perinatal. Virtually all cases of HIV transmission can be attributed to these exposure categories. Transmission rates from the infected host to the uninfected recipient vary by both mode of transmission and the specific circumstances
.
A. MODES OF TRANSMISSION
1- Sexual transmission of HIV from an infected partner to an uninfected partner can occur through male-to-female, female-to-male, male-to-male, and female-to-female sexual contact. Worldwide, sexual transmission of HIV is the predominant mode of transmission.
2- Parenteral transmission of HIV has occurred in recipients of blood and blood products, through transfusion of blood (estimated 95% risk of infection from transfusion of a single unit of HIV-infected whole blood [CDC, 1998a]) or clotting factors, in intravenous or injection drug users through the sharing of needles (approximately 0.67% risk per exposure [Kaplan, 1992]), in health care workers through needle sticks (approximately 0.3–0.4% risk per exposure, depending on the size and location of the inoculum [Updated PHS guidelines, 2001]), and, less commonly, mucous membrane exposure (0.09% risk per exposure (Updated PHS guidelines, 2001).
3- Perinatal transmission can occur in utero, during labor and delivery, or post-partum through breast-feeding (Gwinn, 1996). Perinatal transmission rates average 25–30% (Blanche, 1989) overall in the absence of intervention, but vary by maternal stage of disease, use of antiretroviral therapy, duration of ruptured membranes, practice of breast-feeding, and other factors. In the United States as of December 2001, 91% of cumulative pediatric AIDS cases were attributed to perinatal transmission (CDC, 2002). More information on perinatal transmission can be found in Chapter VII on HIV and Reproduction.
B-FACTORS AFFECTING TRANSMISSION.
1- Mutation of chemokine-receptor gene.
2- Late stage of HIV infection.
3- Primary HIV infection.
4- Anti-retroviral therapy.
5- Local infection.
6- Method of contraception.
A- Barrier decrease Infectiousness and Susceptibility.
B- Spermicidal agents.
C- Intrauterine devices.
7- Factors that lower PH cervix of vagina that decrease HIV Concentration In Genital Secretions and Infectiousness.
8- Immune activation which increase Infectiousness and Susceptibility.
9- Genital tract trauma that increase Infectiousness.
10- Pregnancy increase HIV Concentration in Genital Secretions and Infectiousness.
.
A. MODES OF TRANSMISSION
1- Sexual transmission of HIV from an infected partner to an uninfected partner can occur through male-to-female, female-to-male, male-to-male, and female-to-female sexual contact. Worldwide, sexual transmission of HIV is the predominant mode of transmission.
2- Parenteral transmission of HIV has occurred in recipients of blood and blood products, through transfusion of blood (estimated 95% risk of infection from transfusion of a single unit of HIV-infected whole blood [CDC, 1998a]) or clotting factors, in intravenous or injection drug users through the sharing of needles (approximately 0.67% risk per exposure [Kaplan, 1992]), in health care workers through needle sticks (approximately 0.3–0.4% risk per exposure, depending on the size and location of the inoculum [Updated PHS guidelines, 2001]), and, less commonly, mucous membrane exposure (0.09% risk per exposure (Updated PHS guidelines, 2001).
3- Perinatal transmission can occur in utero, during labor and delivery, or post-partum through breast-feeding (Gwinn, 1996). Perinatal transmission rates average 25–30% (Blanche, 1989) overall in the absence of intervention, but vary by maternal stage of disease, use of antiretroviral therapy, duration of ruptured membranes, practice of breast-feeding, and other factors. In the United States as of December 2001, 91% of cumulative pediatric AIDS cases were attributed to perinatal transmission (CDC, 2002). More information on perinatal transmission can be found in Chapter VII on HIV and Reproduction.
B-FACTORS AFFECTING TRANSMISSION.
1- Mutation of chemokine-receptor gene.
2- Late stage of HIV infection.
3- Primary HIV infection.
4- Anti-retroviral therapy.
5- Local infection.
6- Method of contraception.
A- Barrier decrease Infectiousness and Susceptibility.
B- Spermicidal agents.
C- Intrauterine devices.
7- Factors that lower PH cervix of vagina that decrease HIV Concentration In Genital Secretions and Infectiousness.
8- Immune activation which increase Infectiousness and Susceptibility.
9- Genital tract trauma that increase Infectiousness.
10- Pregnancy increase HIV Concentration in Genital Secretions and Infectiousness.
HIV
The successful introduction and spread of the human immune-deficiency virus (HIV) into the global human population has occurred for many reasons. The discovery and widespread use of penicillin and other
antibiotics meant that there was treatment and cure for most sexually transmitted infections. The existence of these new drugs changed how people perceived risks associated with sexual activity. The development of hormonal contraceptives hastened the pace of change in sexual practices, as prevention of pregnancy without barrier methods became a possibility. Lifestyles were also changing: people were moving into regions that were previously uninhabited by man and long-distance travel became easier and much more common, allowing for greater social migration and sexual mixing. Although the virus may have been first introduced to humans earlier in the 20th century (most likely contracted from infected animals), it was in the 1970s that wider dissemination occurred.
For industrialized countries, the first evidence of the AIDS epidemic was among groups of individuals who shared a common exposure risk. In the United States, sexually active homosexual men were among the first to present with manifestations of HIV disease, followed by recipients of blood or blood products, then injection drug users, and ultimately, children of mothers at risk. Women have represented an increasing proportion of reported AIDS cases in the United States, accounting for 26% of adult cases in 2001 (CDC, 2002). Seventy-eight percent of AIDS cases in women are in African Americans and Hispanics, as compared with 52% of cases in men.
In developing countries, the AIDS epidemic manifested quite differently, both because the signs and symptoms were harder to distinguish from competing causes of morbidity and mortality, and because the epidemic was more generalized, instead of seemingly limited to certain “high-risk” groups. Worldwide, women now represent 50% of all adults living with HIV and AIDS (Table 1-1), and this proportion had been steadily increasing over time (UNAIDS, 2002).
This chapter reviews the epidemiology of HIV/AIDS, beginning with how HIV is transmitted and the variables involved; the natural history of HIV infection in women — both without treatment and in the era of highly active antiretroviral therapy (HAART), and concludes with future issues regarding the HIV/AIDS epidemic
antibiotics meant that there was treatment and cure for most sexually transmitted infections. The existence of these new drugs changed how people perceived risks associated with sexual activity. The development of hormonal contraceptives hastened the pace of change in sexual practices, as prevention of pregnancy without barrier methods became a possibility. Lifestyles were also changing: people were moving into regions that were previously uninhabited by man and long-distance travel became easier and much more common, allowing for greater social migration and sexual mixing. Although the virus may have been first introduced to humans earlier in the 20th century (most likely contracted from infected animals), it was in the 1970s that wider dissemination occurred.
For industrialized countries, the first evidence of the AIDS epidemic was among groups of individuals who shared a common exposure risk. In the United States, sexually active homosexual men were among the first to present with manifestations of HIV disease, followed by recipients of blood or blood products, then injection drug users, and ultimately, children of mothers at risk. Women have represented an increasing proportion of reported AIDS cases in the United States, accounting for 26% of adult cases in 2001 (CDC, 2002). Seventy-eight percent of AIDS cases in women are in African Americans and Hispanics, as compared with 52% of cases in men.
In developing countries, the AIDS epidemic manifested quite differently, both because the signs and symptoms were harder to distinguish from competing causes of morbidity and mortality, and because the epidemic was more generalized, instead of seemingly limited to certain “high-risk” groups. Worldwide, women now represent 50% of all adults living with HIV and AIDS (Table 1-1), and this proportion had been steadily increasing over time (UNAIDS, 2002).
This chapter reviews the epidemiology of HIV/AIDS, beginning with how HIV is transmitted and the variables involved; the natural history of HIV infection in women — both without treatment and in the era of highly active antiretroviral therapy (HAART), and concludes with future issues regarding the HIV/AIDS epidemic
Subscribe to:
Posts (Atom)